Recently, actress Hayden Panettiere has drawn much needed light to a normally silent and lonely disorder, postpartum depression. Hayden says: “…you don’t realize how broad of a spectrum you can really experience [postpartum depression] on. It’s something that needs to be talked about. Women need to know that they’re not alone, and that it does heal.” Many women have gained courage from her example, including myself. She has not only brought courage to others, but has begun a conversation regarding the myriad of ways postpartum depression can be experienced. Everyone’s experience is different, but it doesn’t make anyone’s experience less real. I was able to recognize the signs of postpartum depression in myself, but many women may not know what to look for and may not understand the many different forms that perinatal mood disorders can take.
A few months ago, I was able to put together a survey to get a more real view of postpartum illnesses. I want to express my gratitude and thanks to many of our caring, wonderful readers. I was blown away by the love and support found in the over one hundred responses and I will be drawing on many of the thoughts you expressed throughout my post. Thank you to all who shared your personal stories or thoughts of friends and family members – you truly inspired me. To start off, I have put together some frequently asked questions regarding postpartum depression and some answers that may surprise you!
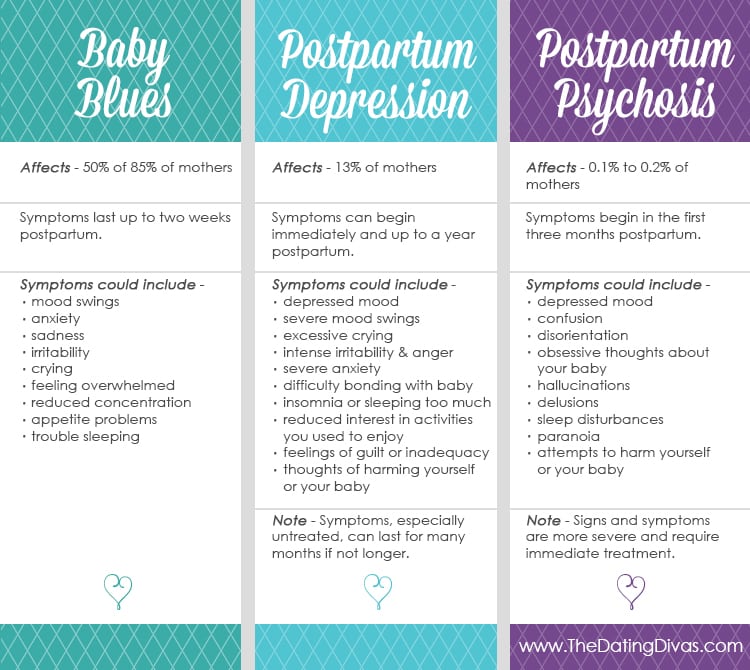
What is a perinatal mood disorder (PMD)? According to a support website called Mother Reach, perinatal mood & anxiety disorder “refers to a group of disorders that includes depression, anxiety, panic, obsessive-compulsive disorder, and bipolar disorder, that occur during pregnancy or the postpartum period. Men can also experience emotional difficulty before or after a baby is born.” How common are perinatal mood disorders? They may be more common than you realize. Baby blues, which occur mostly in the first few weeks after the baby is born, can affect up to 85% of mothers. Postpartum depression affects about 13% of mothers. Postpartum psychosis, on the other hand, is extremely rare and affects 1 in every 1,000 births or about 0.1% of mothers. These numbers may not sound like much, but postpartum depression, combined with psychosis and anxiety, affect about every 1 in 8 mothers. If none of these disorders have affected you, they more than likely affect someone you know. (source) Did you know that Baby Blues, Postpartum Depression, and Postpartum Psychosis are all very different illnesses? Postpartum psychosis, although rare, is often confused for postpartum depression. Some mothers may think if they are just unusually depressed or extremely anxious – that they couldn’t have postpartum depression because they don’t have thoughts to harm their baby. It is important to recognize the signs and differences between these illnesses so that you and your spouse can get the help that you need. (source) What are signs or symptoms for postpartum depression that I, my spouse, or a friend can look for during or after my pregnancy? This list is quite long and, as mentioned, not everyone experiences these disorders in the same way. Some may experience most of these symptoms while others may only experience a few. Many of our survey respondents only selected a few from this list regarding their own personal experience. The five most common symptoms selected on the survey were: depression, anxiety, fatigue, irritability, and hopelessness. Other symptoms include, but are not limited to: anger, guilt, panic attacks, loss of appetite, crying at random moments, unwanted thoughts, eating more than normal, racing thoughts, inability to sit still, rage, delusions/hallucinations, hyperactivity, insomnia, paranoia, rapid mood swings, desire to runaway from everything, suicidal feelings, and thoughts of harming yourself, your baby, or others. When do symptoms start to appear and how long do they last? Just like there are many different perinatal mood disorders, the symptoms can also be experienced differently as well. Symptoms can show up anytime right after birth to up to a year post birth. And symptoms can be experienced anywhere from 2 weeks to up to 3 years. Many of the survey respondents said that they felt symptoms less than 6 months, but most experienced symptoms for more than a year!
For a quick reference the amazing Kristin at CdotLove created this quick and easy table to break down the differences between the three more commonly known PMD. Sources: Mayo Clinic (website link) and University of North Carolina (website link)
I don’t think what I am experiencing is depression or psychosis, but something still feels off? A few of the survey respondents mentioned that they suffered from postpartum anxiety or postpartum obsessive compulsive disorder. These, although less common than PPD, can also affect men and women after the birth of a child and should be taken seriously. You know yourself better than anyone, if something feels off, please speak with your spouse to see what your next steps should be in getting yourself back to your happy, healthy self! I have never dealt with any mental illness in my life/I didn’t experience a perinatal mood disorder with my first baby, so does that mean it will never affect me? Unfortunately the answer is no. Postpartum depression can affect any mother, whether it’s their first baby or their tenth. If you have a previous history with mental illness you may be more susceptible to a perinatal mood disorder, but that does not guarantee you’ll ever experience it. On the other hand, someone who has never dealt with a mental illness may experience some form of perinatal mood disorder with one, some, or even all their childbirths. I feel so alone and scared, where can I turn to for help? First, please reach out to your spouse, remember you are a team and working together through this trial will make all the difference. Next, you can seek help from a medical professional, a family doctor, OB-GYN, midwife, therapist, etc. And don’t forget family members, friends, neighbors, spiritual leaders, and support groups. If the first or even second person you turn to is not helpful, do not give up! There is someone out there who can help you through your postpartum depression, so keep searching! What are some great coping mechanisms I can try to help me get through this? There is no quick fix when it comes to postpartum depression, but there are many things that can help you cope. According to survey respondents, the three most helpful supports were talking to someone, exercise, and medication. Other coping mechanisms include therapy, healthy eating, a routine, sleep, recognizing the issue, honesty, vitamins and supplements, a gratitude journal, support groups, sunshine, essential oils, wearing your baby in a wrap, breastfeeding, discontinuing breastfeeding, couples therapy and running. Remember, everyone is different and not all of these are going to help you or your spouse. They are all great options, but you need to work together to find what helps. When it comes to medication, there are many out there and it may take some looking before finding the right type and dosage. One respondent mentioned they went through five different types of medication before finding the perfect match for them. Don’t give up just because one of the above supports didn’t help you! You deserve to be happy and you will discover the perfect support or mixture of supports that will help you the most!
*Be sure to consult a doctor or psychiatrist before taking any medication. And yes, there are medications that are considered safe while breastfeeding.
– A Message to Those Who Are Struggling –
Whether you are new to motherhood or a veteran, you know that being a mom means doing hard things. And one of the hardest things is asking for help. As moms, we somehow feel that we should be able to do it all, and with a smile on our face. But mental illness is no respecter of persons and is definitely not something many moms plan on. Before the plane takes off before a flight, a flight attendant reviews some safety procedures in case of an emergency. One important message is should the cabin lose pressure, oxygen masks will drop from the overhead area. They then ask that you please place the bag over your own mouth and nose before assisting children. The reason? You can’t help others if you can’t function properly. The oxygen mask helps you breathe so you can in turn help and support others. This is the case for mental illness. If you are suffering from the effects of mental illness, it is harder for you to be there for your children. By first reaching out for help and support for your depression, you will be able to better support and care for your children. My three keys of advice for those personally suffering from postpartum depression or other perinatal mood disorders are: First – You Are Not Alone! Do you hear me?! NEVER! No matter how dark your mind and body feel, you are not alone! There are doctors, nurses, therapists, your spouse, friends, neighbors, and support groups, both in person and on social media, that are here to help you! You may be surprised how many moms have been where you are. You will get through this, and there will be people to help you every step of the way, as long as you follow my second word of advice! Second – Get Help! Don’t wait! As soon as you recognize the signs, reach out. I completely understand how hard it is to express the darkness you feel, especially if people don’t respond well. But don’t give up! Keep reaching out, find someone to talk to! Some friends may not understand, and if you need to take a break from those friendships for a while, remember you are focusing on you and your family. If a doctor is unhelpful or causes you stress, find a new one – you are not forced to work with that one doctor. In fact, one of our survey respondents moved to a different town in order to receive the help she deserved. It may take time, but getting the best help for you is the most important thing. Don’t be ashamed if medication needs to be taken or if you need to meet with a therapist. And if your spouse seems unhelpful, follow my third word of advice. Third – Patience! Number one, have patience with yourself. You didn’t ask for this and, unfortunately, you can’t just wish it away. You are in for a battle and some days are going to be worse than others. Be realistic with your goals. One piece of advice that I have found helpful, is to take this battle one hour at a time. You can set some long term goals, but try and just focus on the hour in front of you. One hour do laundry, next hour play a game/watch a movie with your kids, next hour go for a walk, another hour reach out to a friend, etc. until all of a sudden you are busy, and the day is done. Number two, have patience with your spouse. They are just as confused and lost as you are. If you or they have never dealt with mental illness, they may be lost in a sea of confusion. Try and communicate the best you can with them. Definitely let them know what you are going through – they are your number one source for support. If you want support, you must have enough trust to let them see the darkness affecting you. Men sometimes like to fix things right away and with mental illnes,s that can’t be done, so give them something small that can help you. My husband and I set up a plan that if he comes home to a messy house and a teary eyed wife, he grabs my running shoes and kicks me out the door for a run. While I’m gone, he helps make dinner. We both know that this won’t make my depression go away, but it helps in that moment. This plan works for us, but we had to talk and get to a point of understanding. You can get there with your spouse, as well. A few of the survey respondents included the idea that therapists can be great mediators; with whom both spouses are able to express true feelings and arrive at an understanding. Don’t focus on the stigma surrounding couple’s therapy. Remember the most important thing, you and your health!
– A Note to the Spouse –
Some of the survey respondents expressed the desire to support a spouse, friend, or family member, and didn’t know where to obtain advice. Well, here is a great place to start!
Look for signs: You may think that your spouse is immune to mental illness. It is important to look for signs. They may not recognize that depression has hit them or, if they do, they may be afraid to bring it up in fear that you may judge them. Understand that this is not something your spouse chose to have happen and they cannot just ‘snap out of it.’ Although time will help heal them, in this moment they need your love and support more than ever! Review the list above of possible symptoms and note anything out of character in your spouse. Communication and patience: I cannot stress enough the importance of communication. This is a difficult time for everyone, but good communication will help! Listen to your spouse, really listen. Don’t discredit any thought or feeling. If they casually bring up depression or anxiety, and try to brush it off, don’t forget about it – take it seriously and follow up with them. Ask them how you can best help. If they have a hard time thinking of ideas, create a list of ideas and go over it with them. Ideas could include handling some of the chores, allowing them to get some alone time, taking them out on a date, setting up doctor or therapy appointments, cooking a meal, pushing them to workout, etc. Remember, there is no quick fix and the problem isn’t just going to go away because you want it to, or because you tried one coping mechanism. You are both in this for the long haul – being patient and understanding will make a world of difference. Help them seek help: If your spouse is unable to seek help on their own, do it for them. Make the call, take them to the doctor or therapist. Ignore the protests (but always communicate!). Getting professional help is exactly that, help! If you broke your arm, would you refuse to go to the doctor? Would you look at this broken limb as a personal failure and just live with the pain? Would you just ‘walk it off’ and hope that the pain will subside and the break will eventually just go away? Of course not, mental illness is no different and requires treatment to heal. Get help for yourself: No one expects you to shoulder all of this alone. Be sure to take time for you and your spouse. If you feel yourself slipping down into depression, be sure to speak up.
Here are some other great thoughts for spouses and friends from some of the survey respondents:
“Check in on her. Hold the baby so she can have a rest. Ask how she is doing. Give her an opening to express how she is feeling and make sure to follow-up.” “Make sure you check on new mothers and try to help in anyway you can!” “Read up on [your spouse’s] specific illness to gain a better understanding.” “Be kind and supportive, even if you don’t understand it.” “It’s no fun for us too. Don’t judge us too harshly, we don’t know why we are acting the way we are either.” “The biggest thing to understand is that there really are good days and bad days, and talking about it with anyone can be difficult because we do love our babies. Sometimes we just need someone to say they understand that it is hard.”
– My Personal Story of Postpartum Depression –
Since the day after my baby girl arrived, I have woken up with a dark heaviness. I have dealt with depression much of my life so I recognized the signs of postpartum depression pretty quickly. I kept waiting for this particular depressive episode to disappear, thinking it was just more of my normal funk. But as the months have passed, the depression has not gone away. It has become my constant companion. Some days are worse than others. My husband has journeyed this path with me, like a knight in shining armor, and I count this blessing every day as I know many aren’t as lucky. Many days I barely have the strength to rise out of bed, but somehow I do and with my husband’s support, I will be running a half-marathon soon! But running is only part of how I have learned to cope. On a particularly dark day a few months back I finally reached out to some friends and I realized I had a much larger support network than I realized. And that is where the idea for this post was born. The AMAZING Tara Carson somehow knew just what I needed. I’m a worker. I like to have projects and to-do lists to focus on and this was the perfect one! Not only could writing this post help me persevere through my own postpartum depression, but maybe, just maybe, it could help someone else too! Through my research, I discovered an amazing website, The Emily Effect. It was put together in honor of a mother who lost her life during her fight with postpartum depression. On this website, they have an area where you can submit your story of dealing with perinatal mood disorders! There are already some amazing stories posted, so please follow this link and be inspired – maybe even share your own journey! I was so inspired reading through the survey responses that I realized that this is what so many of us need – to know we truly aren’t alone, that others are fighting the good fight too, and that many have come out on top! So no matter if it is a work in progress or a championing success, please share your story! You never know who it will touch and who will gain the courage to seek help! Writing this post was a difficult journey. Ironically, many days I was too depressed to sit down and put my thoughts together – but I often thought of the many readers who said they were looking forward to this article, and of my many friends who encouraged me. Sometimes I feel we pass through personal trials to help others, and if this article helps just one other person, I will understand, even just slightly, why I have been given this dark journey to pass through. I have only barely touched the tip of the iceberg in regards to perinatal mood disorders, including postpartum depression and postpartum psychosis. There are a lot of other disorders or conditions you may be suffering from, including anxiety, post-traumatic stress disorder, obsessive compulsive disorder, separation anxiety, and antenatal depression (depression during pregnancy). If you are suffering in any way, please seek help!
I hope that you and your spouse can find the help and light you need at this dark time. Don’t give up! Keep fighting the good fight. I am certain the sun will come out tomorrow, no matter the rain clouds we endure now. There is always hope! As one amazing survey respondent stated: “Girl, you are not alone! Never! We are all in this together! Carry on, warrior! We can do hard things!” *IMPORTANT NOTE – This article is in no way professional medical advice. If you think you, a spouse, or a friend is suffering, please seek help! Medical professionals are the only ones who can diagnosis and prescribe medication. Other Helpful Links and Resources:
Postpartum Progress Website Postpartum Depression – When Your Doctor Won’t Listen 14 Things People Should Know about Postpartum Depression The Pregnancy and Postpartum Anxiety Workbook This Isn’t What I Expected: Overcoming Postpartum Depression
Some of our other posts that might be helpful are Marriage After Baby and Helping a Spouse with Depression. We also have an amazing Reclaim Your Marriage Program that helps bring you and your spouse back together during, and after, this difficult trial.